Lung tests sit at the intersection of clinical assessment and personal health monitoring. They are not just about confirming a disease label; they are about understanding how well the lungs move air, how efficiently oxygen passes into the blood, and how conditions like asthma, COPD, or restrictive disorders shape everyday breathing. In recent years the landscape has widened from traditional clinic visits to home friendly devices and digital platforms that connect patients with clinicians in real time. This evolution is changing how individuals track their lung health, how clinicians detect changes early, and how researchers gather data for better treatments.
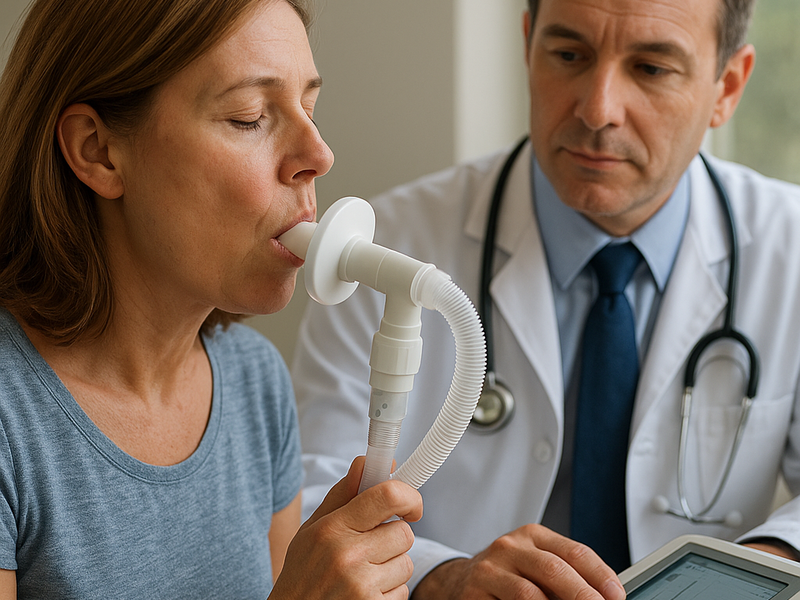
The most common lung test is spirometry, a procedure that measures how much air a person can exhale and how quickly. During a spirometry test the patient inhales fully and then exhales into a mouthpiece as forcefully and completely as possible. The test captures two key numbers: the volume of air exhaled and the rate at which it leaves the lungs. Clinicians look at the Forced Expiratory Volume in a short period, often expressed as FE V one, and the Forced Vital Capacity, FVC. The ratio between these figures helps distinguish obstructive from restrictive patterns. While spirometry has long been the workhorse of respiratory diagnostics, it is only one part of the picture. Other tests, such as diffusing capacity for carbon monoxide, which evaluates how well gases move from the lungs into the blood, and plethysmography, which assesses lung volumes within a sealed chamber, add layers of detail for complex cases.
In practice, lung testing spans multiple settings and purposes. Primary care clinics routinely use spirometry to assess wheeze, chronic cough, and breathing limitations. Hospitals employ comprehensive pulmonary function testing suites that combine several measurements to provide a full picture of lung mechanics. For patients with asthma or COPD, regular testing helps gauge response to therapy and to detect early signs of worsening control. Athletes and fitness enthusiasts increasingly seek lung function data to tailor training and recovery, while preoperative assessments ensure that individuals are fit for surgery. A growing group of patients uses home devices to perform periodic checks, share results with their clinicians, and participate in remote management programs. The shift toward digital health means that data from a home spirometer can be uploaded to a secure platform, replayed in clinician review, and integrated with other health information.
The market presents a spectrum of options, from purpose built clinic instruments to consumer friendly devices and apps. For clinics and hospitals, brands like Vitalograph, COSMED, and MIR Diagnostics have long supplied robust, calibrated spirometers designed for repeated daily use around the world. Vitalograph focuses on user friendly devices that support rapid testing, strong data management, and reliable calibration procedures. COSMED offers high end, research grade systems that deliver precise lung function data and are widely used in pulmonary labs as well as sports science facilities. MIR Diagnostics, with its Vyntus line, emphasizes accuracy and versatility across a range of pulmonary measurements, including spirometry and gas analysis, for clinical and academic settings. These brands are commonly chosen by health systems and clinics that require durable equipment, centralized data, and professional service networks.